
Autoimmune Issues? These Herbs Might Just Leaf You Feeling Better
The Growing Interest in Natural Autoimmune Support
Herbs for autoimmune disease are becoming increasingly popular among patients seeking natural alternatives to conventional treatments. As autoimmune conditions continue to rise globally - with annual increases ranging from 3.7% to 7.1% across different disease categories - more people are exploring herbal remedies to manage their symptoms and support their immune systems.
Quick Answer: Best Herbs for Autoimmune Disease
Immunomodulating herbs (help balance immune response): Chang Shan, Panax Ginseng, Turmeric, Boswellia
Anti-inflammatory herbs: Ginger, Licorice, Reishi mushroom
Herbs to AVOID (may trigger flares): Spirulina, Echinacea, Alfalfa, Chlorella, Elderberry
Here's what makes this topic so complex: your immune system isn't simply "weak" when you have an autoimmune condition - it's overactive and confused. Research shows that 35-69% of dermatology patients use complementary and alternative medicine, often without realizing that some "immune-boosting" herbs can actually make autoimmune symptoms worse.
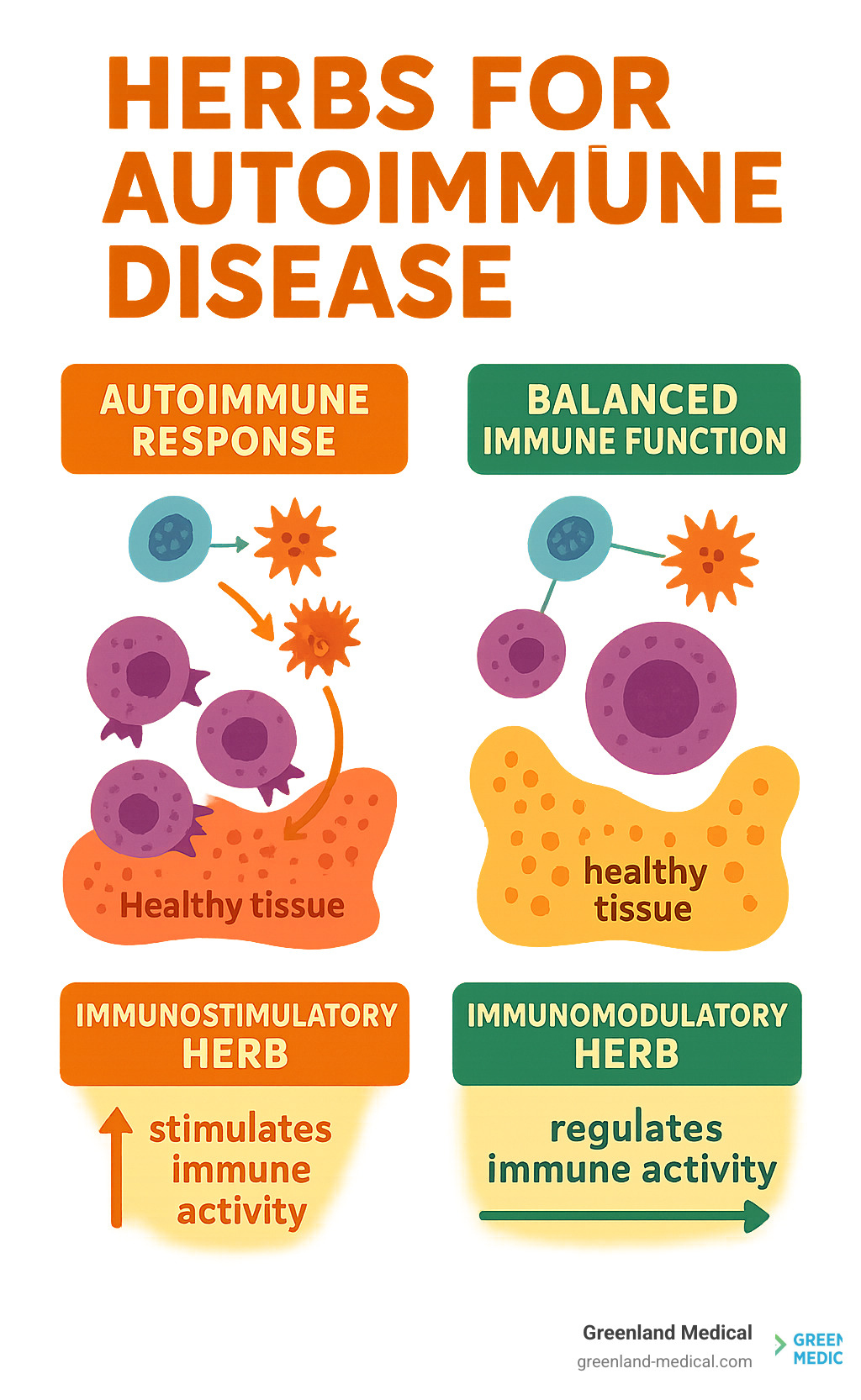
The key difference lies in understanding immunomodulation versus immunostimulation. While immunostimulatory herbs like Echinacea might help healthy people fight off a cold, they can trigger dangerous flares in autoimmune patients by further activating an already hyperactive immune system.
I'm Dr Andrew Greenland, a functional medicine practitioner who has spent years helping patients steer the complex world of herbs for autoimmune disease through personalized, root-cause approaches. My experience with the Bredesen Protocol and chronic inflammatory conditions has shown me that the right herbal strategy - combined with proper medical oversight - can be transformative for autoimmune patients when applied correctly.
The Immune System's Balancing Act: How Herbs Can Help or Harm
When we talk about the immune system, it's easy to picture a valiant knight tirelessly defending the body. But in autoimmune conditions, that knight gets a bit confused and starts attacking its own kingdom. This isn't a problem of weakness, but rather a profound imbalance. Our goal with herbs for autoimmune disease is not to "boost" this overzealous knight, but to help it regain its sense of direction and calm down.
This brings us to a crucial distinction: immunomodulators versus immunostimulants. Immunomodulators are like skilled diplomats; they help bring balance and harmony to the immune system. They can dial down an overactive response or gently nudge a sluggish one into action, depending on what's needed. Immunostimulants, on the other hand, are like a cheerleading squad with megaphones; they indiscriminately amp up immune activity. While fantastic for a healthy immune system facing an infection, this can be disastrous for someone whose immune system is already in overdrive and attacking its own tissues.
The immune system operates through a complex network of cells and signaling molecules called cytokines. Imagine these cytokines as tiny messengers that tell immune cells what to do. In autoimmune conditions, there's often an imbalance in these messages, particularly within the T-helper cell subsets, such as the Th1/Th2 paradigm, and an overproduction of pro-inflammatory cytokines. This is why personalization is non-negotiable when considering herbs for autoimmune disease; what helps one person might harm another, depending on their specific immune dysregulation.
Understanding Key Immune Cells and Pathways
To truly understand how herbs for autoimmune disease can help or harm, we need to get a little acquainted with some key players in the immune system.
T-helper cells (Th1, Th2, Th17, Treg): These are like the strategists of the immune system, directing responses. In autoimmunity, there's often an imbalance, such as an overabundance of Th17 cells, which are known to drive inflammation in many autoimmune diseases like multiple sclerosis and rheumatoid arthritis. Our aim is to rebalance these cells.
Natural Killer (NK) cells: These are the immune system's rapid response team, capable of destroying infected or cancerous cells without prior activation. While essential for fighting off viruses, an increase in NK cell activity can be problematic in autoimmune conditions. For example, a pilot study showed a significant 40% average increase in NK cell activity in healthy patients who consumed Immulina® (a Spirulina extract) for just seven days. While this might sound good for general immunity, in an autoimmune context, it's like adding fuel to an already raging fire.
Pro-inflammatory cytokines (TNF-α, IL-1β, IL-6, IFN-γ): These are the alarm signals that trigger and sustain inflammation. In autoimmune conditions, these messengers are often shouting too loudly, leading to tissue damage. Many beneficial herbs for autoimmune disease work by dampening these inflammatory signals.
Perforin: This is a protein released by NK cells and cytotoxic T-cells, which creates pores in target cells, leading to their destruction. The same Immulina® (Spirulina) study also found that a 400 mg dose led to a 75% increase in mRNA expression of perforin. Again, in a healthy individual, this is a sign of robust immune response. In someone with autoimmunity, this heightened destructive capacity can contribute to the body attacking its own cells.
Immune system regulation: The ultimate goal is to restore balance. Immunomodulatory herbs for autoimmune disease work by influencing various pathways, such as NF-κB and MAPK, which control gene expression related to inflammation and immune cell function. They don't just suppress the immune system but rather guide it back to a state of equilibrium.
Promising Immunomodulating Herbs for Autoimmune Disease

Here's where things get exciting. After understanding how our immune system can go haywire, let's explore some herbs for autoimmune disease that actually show promise in bringing balance back to the chaos. These aren't your typical "immune-boosting" herbs - they're more like skilled negotiators who help calm down an overactive immune response.
The key word here is modulation, not stimulation. Think of these herbs as gentle guides that help your immune system remember how to behave properly, rather than cheerleaders encouraging it to work even harder. While the research on these herbs is genuinely promising, I want to be upfront: we need more human trials to fully understand their potential and safety profiles.
Chang Shan (Dichroa febrifuga): A Traditional Root with Modern Potential
Sometimes the most exciting findies come from looking at ancient wisdom through a modern lens. Chang Shan, a root used in Traditional Chinese Medicine for over 2,000 years, is having its moment in the spotlight - and for good reason.
Researchers at Harvard School of Medicine finded something remarkable about this humble root. It contains a compound called halofuginone (HF) that does something quite clever: it specifically targets the troublemaker immune cells called Th17 cells without bothering the helpful ones your body actually needs.
Here's how it works: HF tricks these rogue Th17 cells into thinking they're starving by activating something called the amino-acid starvation response. These cells basically shut down their inflammatory activity and stop attacking your own tissues. Meanwhile, your other T-cells - the ones that protect you from real threats - keep working just fine.
This selective approach is huge for herbs for autoimmune disease because most conventional treatments act like a sledgehammer, suppressing your entire immune system and leaving you vulnerable to infections. Chang Shan is more like a precision tool.
Early research suggests potential benefits for conditions like scleroderma and multiple sclerosis. As researcher Malcolm Whitman noted, "This compound could inspire novel therapeutic approaches to a variety of autoimmune disorders." The research even hints at applications for dental autoimmune conditions, as discussed in this research on this Chinese herb for autoimmune disorders.
Panax Ginseng: The Adaptogenic Approach
If Chang Shan is the precision tool, then Panax ginseng is the wise diplomat. Known as the "king of herbs," ginseng belongs to a special category called adaptogens - substances that help your body adapt to stress and maintain balance, no matter what's thrown at it.
What makes ginseng fascinating for autoimmune conditions is that it doesn't just push your immune system in one direction. Instead, its active compounds called ginsenosides work like a thermostat, turning down inflammation when it's too high and supporting function when it's too low.
The research on ginseng for autoimmune conditions is genuinely impressive. In multiple sclerosis studies, 86% of patients (52 out of 60) who took ginseng for three months reported less fatigue and better quality of life. For inflammatory bowel disease, ginseng appears to protect the intestinal barrier while calming inflammation. In rheumatoid arthritis models, it helps balance those troublesome Th17 cells we talked about earlier.
One important detail: not all ginseng is created equal. Red ginseng - which is steamed and dried - often shows stronger therapeutic effects with fewer side effects compared to fresh or white ginseng. Some research even suggests that fermented ginseng might be even more beneficial.
You can dive deeper into the research here: Panax ginseng as a candidate for autoimmune disease. The scientific community is calling it a potential "panacea" for autoimmune conditions, though more human trials are definitely needed to fully open up its potential.
The beauty of these immunomodulating herbs for autoimmune disease is their intelligence - they seem to know exactly what your immune system needs to find its way back to balance.
Caution Advised: When "Immune-Boosting" Herbs Backfire
Here's where things get tricky with herbs for autoimmune disease. While we've explored some promising immunomodulating options, there's a whole category of popular "immune-boosting" herbs that can actually make autoimmune conditions much worse. It's like the difference between a skilled therapist helping someone work through their anger versus someone shouting "get angrier!" at an already furious person.
At Greenland Medical, I see this scenario play out regularly. A well-meaning patient reads about the immune-boosting benefits of Spirulina or Echinacea, starts taking them to "support their health," and then experiences a mysterious flare in their autoimmune symptoms. They often don't connect the dots, thinking their condition is just getting worse naturally.
The reality is that when your immune system is already attacking your own tissues, adding an immunostimulant is like throwing fuel on a fire. This is especially dangerous for autoimmune skin conditions like dermatomyositis, pemphigus, and lupus erythematosus, where the connection between these supplements and disease flares has been well-documented in medical literature.
The supplement industry reached $11.3 billion in sales in 2020, with immune-supportive products being particularly popular. Unfortunately, most people don't realize that "immune support" can mean very different things depending on whether your immune system needs gentle guidance or is already running wild.
The Algae Alert: Spirulina, Chlorella, and A. flos-aquae
Blue-green algae like Spirulina and Chlorella have earned "superfood" status in recent years, marketed as natural ways to boost energy and immunity. For people with autoimmune conditions, however, these supplements can be genuinely dangerous.
The problem lies in their mechanism of action. These algae are powerful NK cell activators. Remember those Natural Killer cells we discussed earlier? They're like your immune system's special forces unit - great for taking out infected cells, but problematic when they're already targeting healthy tissue in autoimmune disease.
A fascinating study on Immulina® (a Spirulina extract) revealed just how potent these effects can be. Healthy volunteers who took just 400 mg daily for seven days experienced a 40% average increase in NK cell activity. Even more concerning, researchers found a 75% increase in perforin expression - that's the protein these cells use to punch holes in their targets.
While this might sound impressive for general health, it's terrifying if you have an autoimmune condition. Research published on the effects of immunostimulatory herbs on autoimmune skin diseases includes several eye-opening case reports that illustrate this danger perfectly.
One patient developed cutaneous dermatomyositis after taking a supplement containing A. flos-aquae. Another person with previously quiet pemphigus vulgaris experienced a sudden flare after starting Spirulina. Perhaps most telling, researchers found that 47% of dermatomyositis patients who used Spirulina reported disease flares that they could directly link to taking the supplement.
These aren't isolated incidents - they represent a pattern that's becoming increasingly recognized in autoimmune medicine.
Why Echinacea and Alfalfa Need a Second Look for Autoimmune Conditions
Two other herbs that frequently cause problems for autoimmune patients are Echinacea and Alfalfa. Both have strong reputations as health-promoting supplements, which makes their potential dangers particularly insidious.
Echinacea's immunostimulatory effects work by ramping up cytokine production - specifically inflammatory messengers like TNF-alpha, IL-1beta, and IFN-gamma. These are exactly the same inflammatory signals that are already overactive in most autoimmune conditions. It's like adding more megaphones to an already too-loud crowd.
The case reports tell a sobering story. One patient with well-controlled pemphigus vulgaris took Echinacea for a cold and triggered a significant flare. Another developed erythema nodosum after using Echinacea supplements, which resolved when they stopped taking it. In studies of autoimmune skin conditions, patients using similar immunostimulatory herbs experienced flare rates of 50-62%.
Alfalfa presents a different but equally concerning risk through a compound called L-canavanine. This amino acid is chemically similar to arginine, which means your body can accidentally incorporate it into proteins during normal protein synthesis. The result? Your immune system recognizes these "wrong" proteins as foreign and mounts an attack against them.
The connection to lupus is particularly strong and well-documented. Healthy volunteers have developed lupus-like laboratory abnormalities after eating alfalfa seeds. In animal studies, monkeys fed alfalfa sprouts developed a lupus-like syndrome complete with the characteristic skin rash. Human patients have developed symptomatic lupus-like disease after taking alfalfa tablets, and two patients experienced acute dermatomyositis flares after consuming weight loss shakes containing alfalfa.
This evidence is so compelling that the Lupus Foundation specifically advises caution with alfalfa for people with lupus and related conditions.
The most troubling aspect of these supplement-induced flares is that patients often don't recognize the connection. They may interpret the worsening symptoms as natural disease progression, leading them to continue taking the harmful supplement while seeking more aggressive medical treatment for what they perceive as a deteriorating condition.
This is exactly why transparency with your healthcare provider about every supplement you're taking isn't just helpful - it's essential for your safety.
A Smart and Safe Guide to Using Herbs for Autoimmune Disease
Think of using herbs for autoimmune disease like learning to drive a race car - the potential is incredible, but you definitely need an experienced instructor and proper safety measures in place. At Greenland Medical, we've seen the transformative power of the right herbal approach, but we've also witnessed the serious consequences when things go wrong.
The truth is, your autoimmune condition makes you unique. What works beautifully for your friend with rheumatoid arthritis might trigger a devastating flare in your lupus. This isn't a "one-size-fits-all" situation, and that's exactly why professional guidance isn't optional - it's absolutely essential.
Consultation is Mandatory
I can't stress this enough: please don't try to steer herbs for autoimmune disease on your own. Your immune system is already confused and overactive, and adding the wrong herb can be like accidentally hitting the gas pedal instead of the brakes.
Working with a qualified practitioner who understands autoimmune conditions is crucial. Look for someone with specific experience in functional medicine, naturopathy, or clinical herbalism who truly gets the complexity of immune system dysfunction. They'll know which herbs might calm your particular type of immune chaos and, just as importantly, which ones could make things worse.
Disclosing all supplements to your doctor isn't just a nice suggestion - it's a safety must-do. I know it might feel awkward to mention that turmeric supplement or green tea extract, but your medical team needs the complete picture. They can't protect you from dangerous interactions or properly assess your symptoms if they're working with incomplete information.
Many patients worry their doctors will dismiss their interest in natural approaches, but most healthcare providers genuinely want to keep you safe and will appreciate your honesty. If they seem resistant, it's often because they've seen patients get hurt by undisclosed supplements, not because they're against natural medicine entirely.
Questions to Ask Your Healthcare Provider
When you're ready to discuss herbs for autoimmune disease with your healthcare team, come prepared with specific questions that show you're taking this seriously:
Is this herb safe for my specific condition? Your lupus, rheumatoid arthritis, or Hashimoto's each have different patterns of immune dysfunction, and what's safe for one might be dangerous for another.
Could it interact with my medications? This is especially critical if you're taking immunosuppressants, biologics, or blood thinners. Some herb-drug interactions can be life-threatening.
What's a safe dosage for me? The amount that works safely varies enormously based on your size, condition severity, other medications, and individual metabolism.
How will we monitor for problems or benefits? Your practitioner should have a clear plan for tracking your progress, whether through specific lab tests, symptom journals, or regular check-ins.
What warning signs should I watch for? Know exactly what symptoms might indicate a flare or adverse reaction, so you can stop the herb immediately and seek help.
These conversations help ensure you're making informed decisions rather than hoping for the best.
The Future of Herbal Research in Autoimmunity
The field of herbs for autoimmune disease is evolving rapidly, but we're still in the early chapters of this story. While the research on herbs like Chang Shan and Panax ginseng is promising, significant gaps remain that need addressing.
Large-scale clinical trials are desperately needed. Most of our current knowledge comes from small studies, animal research, or traditional use patterns. While these provide valuable insights, we need robust human trials to truly understand optimal dosages, long-term safety, and which patients are most likely to benefit.
Product standardization remains a major challenge. Walk into any health food store, and you'll find dozens of turmeric supplements with wildly different potencies and quality levels. This inconsistency makes it nearly impossible for practitioners to predict results or for patients to know what they're actually taking.
The promise of personalized herbal medicine excites me most. Just as we use individualized approaches like the Bredesen Protocol at Greenland Medical, the future lies in tailoring herbal protocols to each person's unique genetic makeup, gut microbiome, and specific immune dysfunction patterns.
Imagine a world where we can analyze your immune system's particular quirks and design a precise herbal protocol that addresses your exact imbalances. We're not there yet, but we're moving in that direction, combining ancient wisdom with modern precision medicine.
This personalized approach represents the best of both worlds - honoring the traditional knowledge that has guided herbal medicine for thousands of years while applying rigorous scientific methods to ensure safety and effectiveness for each individual patient.
Conclusion: Your Personalized Path to Feeling Better
Throughout this exploration of herbs for autoimmune disease, one truth has emerged crystal clear: these natural remedies are incredibly powerful tools, but they're definitely not a magical cure that works the same for everyone. Your immune system is as unique as your fingerprint, and what helps one person might actually harm another.
We've finded some genuinely exciting possibilities. Chang Shan's ability to selectively target harmful Th17 cells without suppressing your entire immune system is remarkable. Panax Ginseng's adaptogenic wisdom in knowing when to calm things down and when to gently support is equally impressive. But we've also seen the darker side - how innocent-seeming "immune boosters" like Spirulina and Echinacea can send someone with autoimmune disease into a painful flare.
The difference between success and setback lies in understanding one fundamental principle: your immune system isn't broken, it's confused. It doesn't need more stimulation - it needs intelligent guidance back to balance. This is why the immunomodulating approach we've discussed is so different from the typical "boost your immunity" message you see everywhere.
Caution and expertise are absolutely paramount when considering herbs for autoimmune disease. This isn't the time for DIY experiments or following what worked for your friend's cousin. Your autoimmune condition has its own personality, its own triggers, and its own needs. Working with someone who truly understands this complexity isn't just helpful - it's essential for your safety.
At Greenland Medical, we see this personalized, root-cause approach in action every day in our Richmond, Twickenham, and London practices. Rather than simply handing out supplements or suppressing symptoms, we dig deep to understand what's driving your immune system's confusion in the first place. We combine the wisdom of traditional herbal medicine with cutting-edge protocols like the Bredesen Protocol, creating treatment plans that are as unique as you are.
The real value lies in addressing the root causes - whether that's hidden infections, gut imbalances, nutrient deficiencies, or environmental toxins that are keeping your immune system in a state of alarm. When we fix these underlying issues and carefully introduce the right herbal support, the results can be truly transformative.
If you're ready to move beyond the guesswork and start your own personalized journey toward better health, we're here to guide you every step of the way. Because feeling better isn't just about finding the right herb - it's about finding the right approach for your unique body and situation.
