
Food Allergy Test Kits: Hype or Help? An Expert's Take
The At-Home Testing Boom: Promise or Pitfall?
Food allergy test kit options are everywhere now. You can order one online, collect a sample at home, and get results in days—all without stepping into a doctor's office.
Quick Answer: Are At-Home Food Allergy Test Kits Worth It?
For True Allergies (IgE): Blood tests from accredited labs can be helpful for screening, but they're not a replacement for medical diagnosis
For Sensitivities (IgG): Scientific validity is debated; many experts caution against relying solely on these results
For Intolerances: Breath tests for lactose or fructose malabsorption have established clinical use
Bottom Line: Tests can be a useful starting point, but they're not a diagnosis—and they carry risks of false positives and unnecessary food elimination
The appeal is obvious. If you're dealing with unexplained symptoms—chronic bloating, fatigue, skin rashes, brain fog—you want answers. When conventional doctors haven't helped, a simple at-home test sounds like a lifeline.
But here's the uncomfortable truth: not all tests are created equal. Some measure genuine immune responses. Others use methods that lack scientific backing. And even the legitimate tests can be misunderstood, leading to restrictive diets that do more harm than good.
In the UK alone, it's estimated that around 2 million people have a diagnosed food allergy, with many more suffering from intolerances. Add to that an estimated 23% of the global population who will live with three to five undiagnosed food sensitivities their entire lives. That's a lot of people searching for clarity—and a lot of opportunity for companies to sell hope without help.
So how do you separate the signal from the noise?
I'm Dr Andrew Greenland, a dual-trained medical doctor and Certified Functional Medicine Practitioner who specializes in chronic illness and gut health. Over the years, I've reviewed countless food allergy test kit results with patients, and I've seen both the benefits and the pitfalls firsthand.
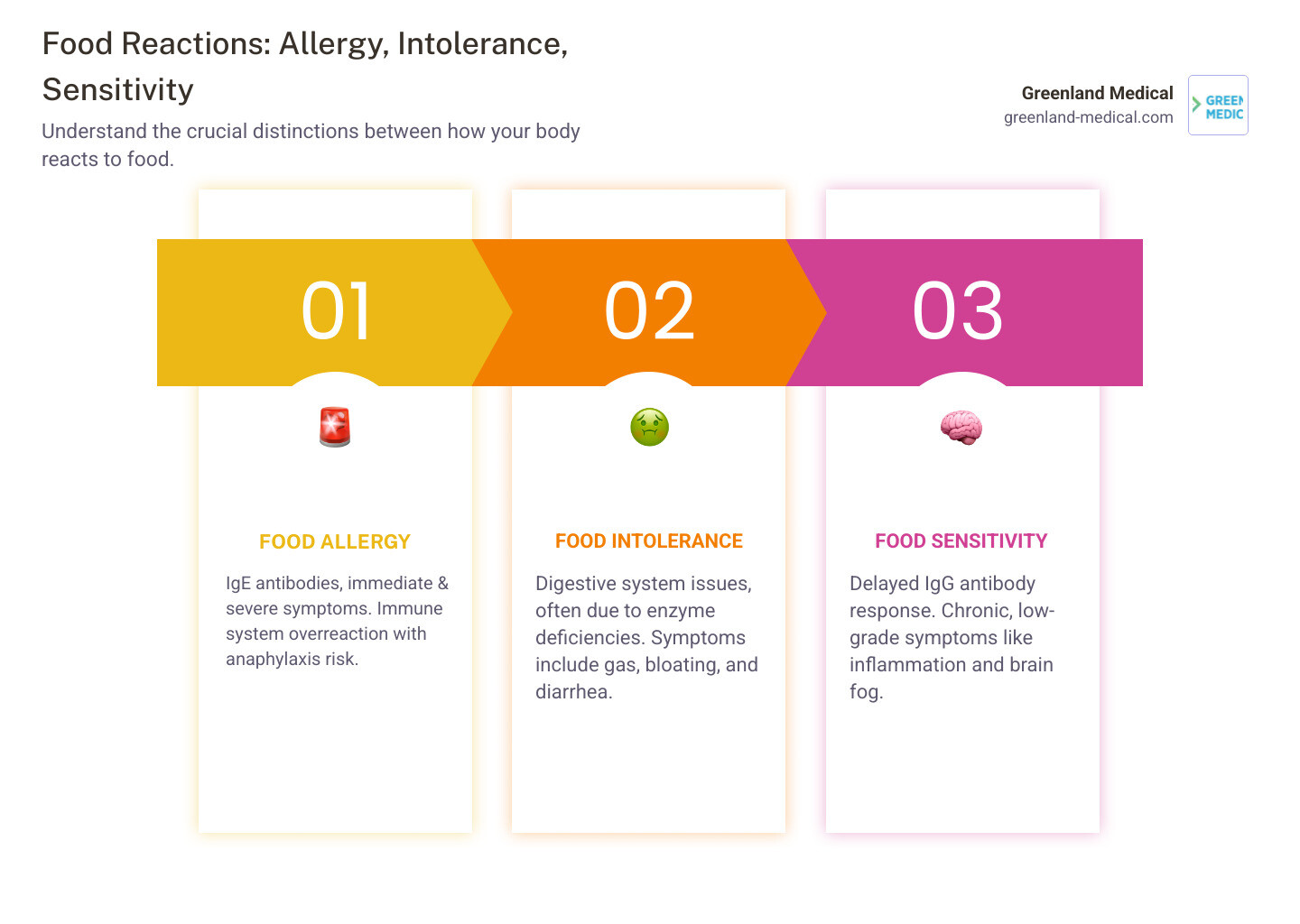
Allergy, Intolerance, or Sensitivity? Understanding Your Body's Reaction
Before you order a food allergy test kit, let's clear up some confusion. People throw around the words "allergy," "intolerance," and "sensitivity" like they're interchangeable. They're not. Understanding the difference isn't just semantics—it's the key to finding real answers instead of chasing ghosts.
Food Allergy: The Immune System's Alarm Bell
A true food allergy is serious business. It's an immediate, full-blown immune system response where your body mistakes a harmless food protein for a dangerous invader. When this happens, your immune system produces specific antibodies called Immunoglobulin E (IgE)—think of them as tiny alarm bells that start screaming the moment they detect the "threat."
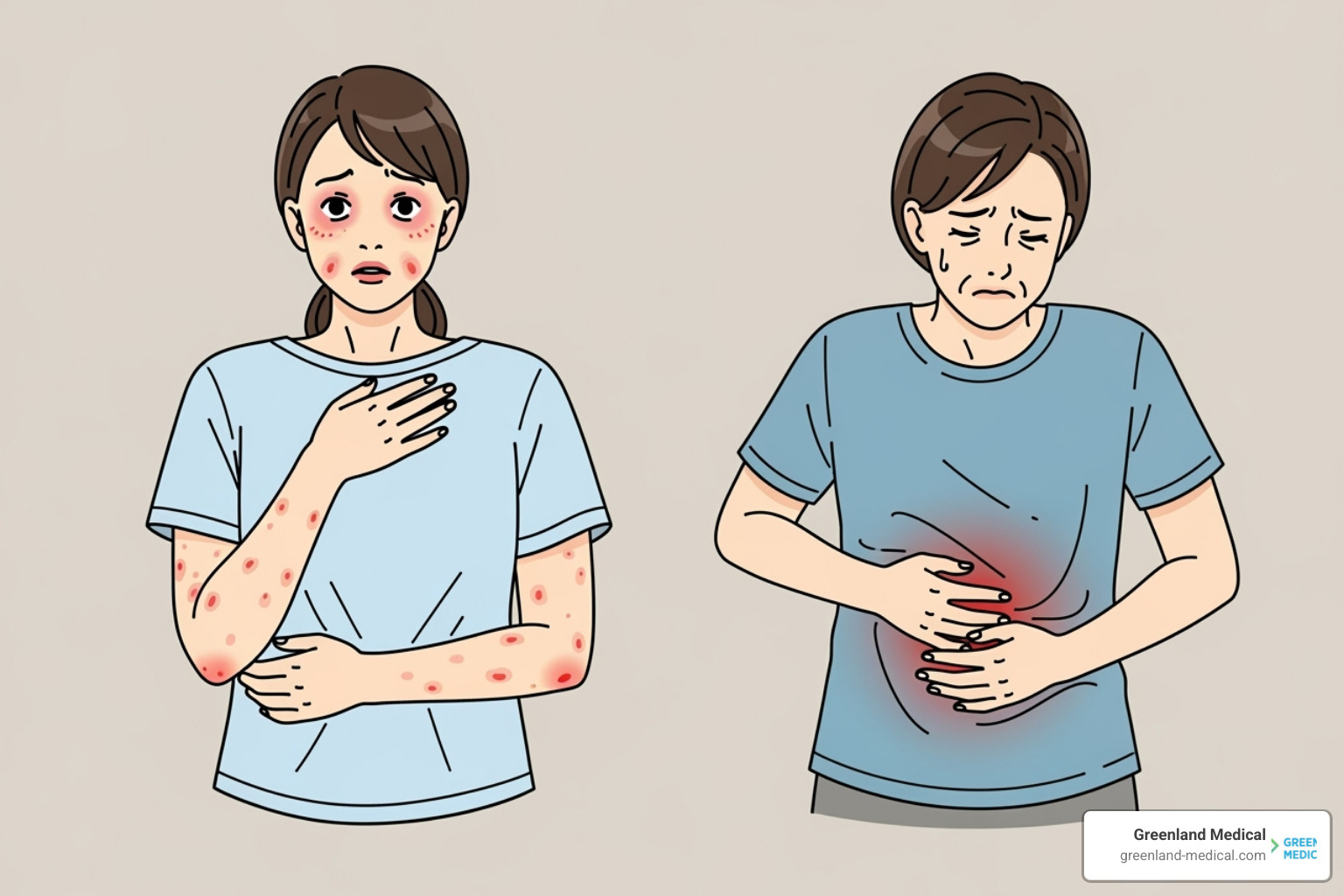
The next time you eat that food, those IgE antibodies trigger the release of histamine and other chemicals throughout your body. The result? Symptoms that appear within minutes to two hours, ranging from uncomfortable to life-threatening.
You might experience hives, itching, or swelling of the lips, face, or tongue. Your mouth might tingle. You could develop wheezing, difficulty breathing, or a tightening in your airways. Some people get stomach pain, vomiting, or rapid pulse. In severe cases, you're looking at anaphylaxis—a full-body reaction that can kill you if not treated immediately with epinephrine.
The usual suspects? Peanuts, tree nuts, milk, eggs, soy, wheat, fish, and shellfish. These are the allergens that require legal labeling in many countries because of how dangerous they can be.
Food Intolerance: A Digestive Disagreement
Food intolerances are less dramatic but still miserable. Unlike allergies, they don't involve your immune system launching an attack. Instead, your digestive system simply can't handle certain food components—usually because you're missing the right enzymes to break them down.
The classic example is lactose intolerance. Your body doesn't produce enough lactase enzyme to digest lactose (the sugar in milk), so it sits in your gut causing trouble. The result? Gas, bloating, abdominal pain, diarrhea—all the fun digestive symptoms that can ruin your day.
These reactions typically happen hours after eating the trigger food, not immediately. They're uncomfortable and frustrating, but they won't send you to the emergency room. Your symptoms stay confined to your digestive tract rather than spreading throughout your body.
Food Sensitivity: The Stealthy Saboteur
This is where things get murky—and where many at-home food allergy test kits focus their attention. Food sensitivities involve a different type of immune response, often mediated by Immunoglobulin G (IgG) antibodies instead of IgE.
Here's the tricky part: symptoms can show up anywhere from a few hours to several days after you eat the trigger food. Try connecting those dots without help. You might eat dairy on Monday and feel brain fog on Wednesday without ever making the connection.
The symptoms tend to be chronic and low-grade rather than acute. We're talking about persistent bloating, nagging fatigue, recurring headaches, stubborn skin issues like eczema or acne, joint pain that won't quit, brain fog that makes you feel like you're thinking through molasses, or mood swings you can't explain. These symptoms create ongoing inflammation in your body, but they're subtle enough that you might just assume this is how life feels.
I need to be straight with you: the medical community is divided on IgG testing. While IgE antibodies clearly indicate allergies, the role of IgG antibodies in causing symptoms is hotly debated. Some experts argue that IgG antibodies simply show you've been exposed to a food, not that you're reacting badly to it. This is why expert opinions on the limitations of IgG testing emphasize caution.
That said, I've seen patients dramatically improve their symptoms by using IgG test results as a starting point for elimination diets. The key word there is starting point—not gospel truth.
The Numbers Tell a Story
While around 2 million people in the UK have a food allergy confirmed by a healthcare professional, many more suffer from intolerances. But here's the kicker: an estimated 23% of the global population lives with three to five undiagnosed food sensitivities their entire lives.
That's a massive gap between people who have answers and people who are suffering without knowing why. Many of those people are walking around with chronic symptoms, cycling through doctors who can't figure out what's wrong, wondering if it's all in their heads.
It's not in your head. But figuring out what's actually happening requires understanding these distinctions. True allergies cause immediate, potentially severe reactions through IgE antibodies. Intolerances create digestive distress because you lack certain enzymes. Sensitivities trigger delayed, chronic symptoms that might involve IgG antibodies—though the science there is still evolving.
A true allergy might show up as swelling and hives within minutes. An intolerance gives you bloating and diarrhea a few hours after eating. A sensitivity might cause fatigue and brain fog two days later, making it nearly impossible to identify without systematic testing or elimination.
This is why at-home tests can be helpful—but only if you understand what they're actually measuring and what their limitations are. Which brings us to our next section.
A Comparison of At-Home Testing Methods
The market is flooded with various at-home food allergy test kit options, each claiming to open up the secrets of your body's reactions to food. But how do they actually work, and more importantly, how reliable are they? Let's break down the most common types you'll encounter.
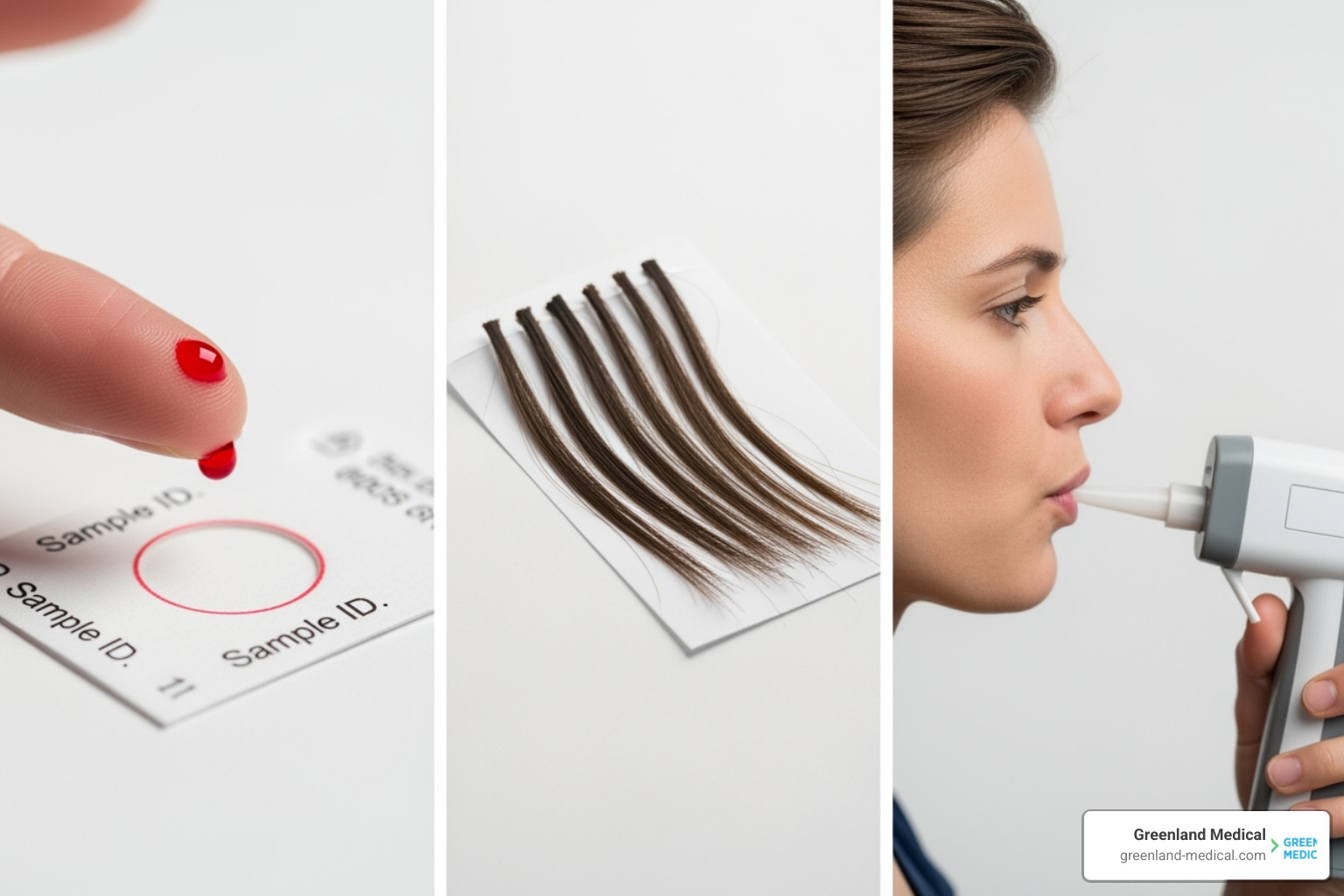
Blood Antibody Tests (IgG/IgE)
This is probably what comes to mind when you think "at-home food allergy test kit." You prick your finger, collect a few drops of blood on a card, mail it to a lab, and wait for your results. Simple enough. But what's actually being measured?
These tests analyze your blood for specific antibodies—either IgE or IgG—depending on what the company is testing for.
IgE blood tests look for the antibodies that trigger true allergic reactions. When done through an accredited lab (we'll talk more about this important credential later), these can be a helpful screening tool. But here's the catch: a positive IgE test doesn't automatically mean you have a clinical allergy. It means you're sensitized—your body has produced IgE antibodies to that food. Whether you'll actually react when you eat it is a different question entirely.
As many experts point out, "A positive test only means you're sensitized. It doesn't mean you're allergic." That's why these results need to be interpreted alongside your actual symptoms and medical history, ideally by a healthcare professional who understands the nuances.
IgG blood tests are where things get more controversial. These measure IgG antibodies, which companies claim indicate food sensitivities—those delayed reactions that cause chronic symptoms like brain fog, fatigue, and digestive issues. Many kits test hundreds of foods using sophisticated-sounding technology, promising to identify the hidden triggers behind your symptoms.
The problem? The scientific community is deeply divided on whether liftd IgG levels actually indicate a problem. Some experts argue that IgG antibodies are simply a normal immune response to foods you eat regularly, not a sign of sensitivity. We'll dig deeper into this debate in the next section.
Breath Tests for Intolerances
If you suspect you have trouble digesting certain sugars—like lactose in milk or fructose in fruit—breath tests are actually a clinically validated option with solid science behind them.
Here's how they work: when your body can't properly absorb certain sugars in your small intestine, they travel to your large intestine where gut bacteria ferment them. This fermentation produces hydrogen and methane gas, which you then exhale. By measuring these gases in your breath after consuming a specific sugar, the test can confirm whether you're malabsorbing it.
These tests are particularly useful for diagnosing lactose intolerance and fructose malabsorption. They're also key for identifying issues with specific FODMAPs—those fermentable carbohydrates that can wreak havoc on people with IBS.
Some at-home devices let you test multiple FODMAPs like lactose, fructose, sorbitol, and inulin, giving you immediate feedback on your breath hydrogen levels. This real-time data can be incredibly helpful for understanding your digestive patterns and guiding dietary changes.
Hair Analysis Tests
Now we enter controversial territory. Some companies offer hair analysis tests, claiming they can identify sensitivities to hundreds—even 600 or more—items just from a few strands of your hair.
The methodology here relies on something called bioresonance technology. Proponents claim that your hair contains energetic frequencies that can be "read" to detect imbalances or sensitivities to various substances, from foods to environmental factors to vitamins. Some companies promise results in as little as five days and use terms like "quantum-certified" to describe their process.
Here's the uncomfortable truth: this approach lacks strong scientific backing. The concept of measuring "energetic frequencies" in hair falls outside our conventional understanding of human physiology and immunology.
Major medical organizations, including the American Academy of Allergy, Asthma & Immunology, don't endorse hair analysis for allergy or sensitivity testing. The reason is simple: IgG antibodies—the markers these tests claim to measure—are only found in blood, not in hair samples. As one testing company that focuses on blood analysis bluntly states, "Hair tests for food intolerances are a waste of money and scientifically unfounded."
I've seen patients come in with hair test results showing sensitivities to dozens of foods, leading to extremely restrictive diets that caused more harm than good. While I respect that people are searching for answers, the scientific consensus simply doesn't support this methodology.
Here's how these three approaches compare:
Test Type Sample Type What It Measures Best For Scientific Validity Blood (IgE) Finger-prick blood IgE antibodies (immediate immune response) Screening for true food allergies High—when done through accredited labs; requires medical interpretation Blood (IgG) Finger-prick blood IgG antibodies (delayed immune response) Identifying potential food sensitivities Controversial—scientific debate about clinical significance Breath Test Breath sample Hydrogen and methane gas from fermentation Diagnosing sugar malabsorption (lactose, fructose, FODMAPs) High—clinically validated for specific intolerances Hair Analysis Hair strands Claimed "energetic frequencies" or bioresonance Various sensitivities (claimed) Low—lacks scientific evidence; not endorsed by medical organizations
The bottom line? Not all at-home tests are created equal. Some have solid science behind them, while others are essentially selling hope without substance. Understanding these differences is crucial before you invest your money—and more importantly, before you make significant dietary changes based on the results.
