
Understanding Borreliosis: A Comprehensive Guide to Lyme Disease
What You Need to Know About Borreliosis Disease
Borreliosis disease, also known as Lyme disease, is a bacterial infection from spirochete bacteria transmitted by infected tick bites. If untreated, it affects the skin, joints, heart, and nervous system.
Key Facts About Borreliosis:
Cause: Borrelia bacteria (primarily Borrelia burgdorferi in North America)
Transmission: Infected black-legged ticks (deer ticks)
Early Signs: Bull's-eye rash (60-80% of cases), fever, fatigue, headache
Treatment: Antibiotics are highly effective when started early
Prevention: Use repellent, wear protective clothing, check for ticks daily
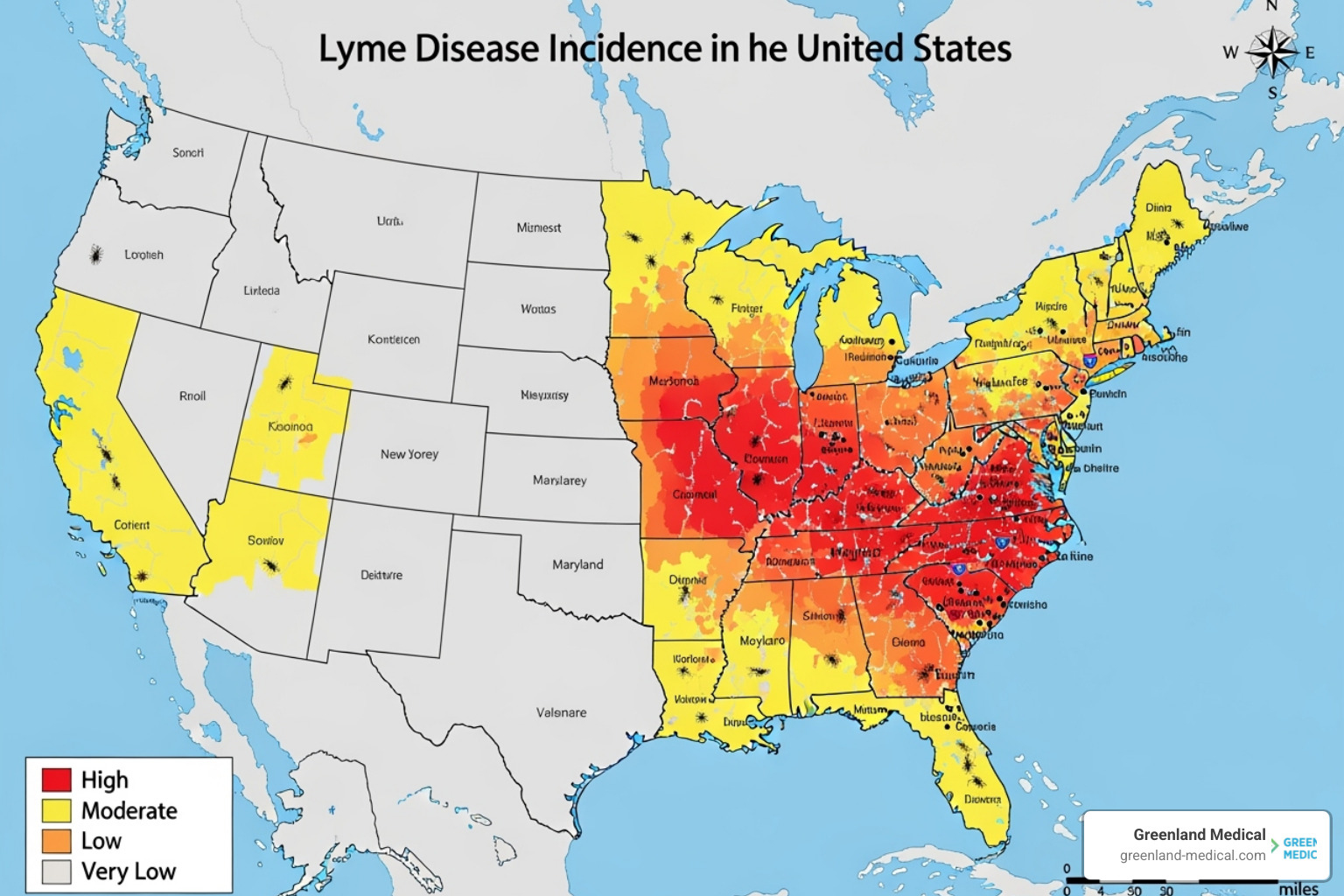
Geographic Risk: Highest in northeastern and upper midwestern United States, parts of Europe and Asia
If untreated, the disease has three stages. Early localized infection (3-30 days post-bite) features the erythema migrans rash. Early disseminated infection (weeks-months later) can cause multiple rashes, facial palsy, and heart problems. Late disseminated infection may cause severe joint pain (Lyme arthritis) and neurological issues.
About 30,000 cases are reported annually in the U.S., but the CDC estimates the actual number may be 12 times higher. Most infections occur in spring and summer when ticks are most active.
Early diagnosis and treatment are crucial - over 80% of patients treated with appropriate antibiotics in the early stages recover completely. However, delayed treatment can lead to more complex, chronic symptoms affecting multiple body systems.
As Dr Andrew Greenland, I've spent years helping patients with complex chronic illnesses, including those struggling with post-treatment symptoms or undiagnosed borreliosis disease cases that conventional medicine often misses. Through functional medicine approaches at Greenland Medical, we address the root causes of persistent symptoms and support the body's natural healing processes.
The Cause, Transmission, and Risk Factors of Borreliosis
Borreliosis disease is caused by spiral-shaped Borrelia bacteria. The main species is Borrelia burgdorferi in North America, while Borrelia afzelii and Borrelia garinii are common in Europe and Asia. These bacteria survive in various hosts, from small mammals and birds to humans.
The journey of Borrelia to a human begins with a tick. Ticks acquire the bacteria by feeding on infected animals. The bacteria multiply in the tick's gut and can be transmitted to a human when the tick feeds again.
The duration of tick attachment is critical for transmission. The bacteria are less likely to spread if the tick is removed within 24 hours. The infection risk rises the longer the tick feeds, making prompt removal a key defense against borreliosis disease.

How Borreliosis is Transmitted by Ticks
The primary vectors for borreliosis disease are ticks belonging to the Ixodes genus, often called "hard ticks." In North America, the black-legged tick (Ixodes scapularis), also known as the deer tick, is the main carrier in the eastern and central United States. On the Pacific Coast, the western black-legged tick (Ixodes pacificus) takes on this role. In Europe, Ixodes ricinus (the castor bean tick or sheep tick) and Ixodes persulcatus are the chief transmitters.
When an infected tick bites a human, the Borrelia spirochetes migrate from the tick's midgut to its salivary glands, a process triggered by the warmth of the blood meal. Once in the salivary glands, the bacteria can be transmitted through the tick's saliva into the human bloodstream. This process typically takes several hours, underscoring the importance of early tick removal.
Scientific research has consistently shown the direct link between tick attachment duration and pathogen transmission. One study, for instance, highlights how pathogen transmission in relation to duration of attachment by Ixodes scapularis ticks affects the likelihood of infection. This evidence reinforces our recommendation: the sooner you remove a tick, the lower your risk of contracting borreliosis disease.
Risk Factors and Geographic Hotspots
Those most at risk for borreliosis disease spend time outdoors in tick-prone environments like wooded or grassy areas. This includes hikers, campers, gardeners, and hunters. The peak season for infection risk is April to October. Immature ticks (nymphs), active in spring and early summer, are tiny and harder to spot, making them a stealthy threat.
Pet owners also face an liftd risk, as pets can bring ticks into the home environment. Regular tick checks on your furry friends are crucial for both their health and yours.
Geographically, borreliosis disease is concentrated in specific regions. In the U.S., high-risk areas include the upper Midwest and the northeastern and mid-Atlantic states. While about 30,000 cases are reported to the CDC annually, some estimates suggest the actual number could be as high as 476,000.
Europe also has a significant burden, with over 200,000 cases treated annually. Central European countries have high tick infection rates, sometimes over 10%. Cases are also reported in parts of Asia.
It's worth noting that climate change is influencing the geographic spread of ticks and, consequently, the incidence of borreliosis disease. As temperatures rise and habitats shift, tick populations are expanding into new areas, bringing the risk of infection with them.
Recognizing the Signs: Symptoms and Stages of Borreliosis Disease
One of the trickiest aspects of borreliosis disease is its varied presentation. Symptoms differ greatly and often appear in stages that can overlap. Some individuals have mild or no early symptoms, so the infection can go unnoticed for months or years. This variability is why borreliosis is often called "the great imitator," as it mimics many other conditions.
While most people experience symptoms, it's also possible to have an asymptomatic infection, meaning you're infected with Borrelia but show no signs of illness. This is why understanding the stages and potential symptoms is so vital for early detection and intervention. We have more detailed information available on Lyme disease symptoms and causes.
Stage 1: Early Localized Infection (3-30 Days)
This stage, 3 to 30 days after a tick bite, is the golden window for effective treatment.
The most distinctive sign of early localized borreliosis is the erythema migrans (EM) rash, which develops in 60-80% of infected individuals. It starts as a small red bump at the bite site and expands, sometimes clearing in the center to form a "bull's-eye." However, not all EM rashes look like a bull's-eye; they can be uniformly red or have atypical shapes. The classic target-like pattern is more common in Europe (in 79% of rashes) than in the US (19%).

Alongside the rash, many people experience flu-like symptoms, even without a cough or runny nose. These include:
Fever and chills
Headache
Fatigue (often profound)
Muscle and joint aches
Swollen lymph nodes
It’s easy to mistake these symptoms for a common cold or flu, especially if you don’t recall a tick bite or don't develop the rash. This is why we always encourage heightened awareness if you've been in tick-prone areas.
Stage 2: Early Disseminated Infection (Weeks to Months)
If borreliosis disease is left untreated, the Borrelia bacteria can spread through the bloodstream, leading to more severe symptoms. This stage typically occurs weeks to months after the initial infection, often 3 to 10 weeks after the bite.
Symptoms in this stage can include:
Multiple rashes: The bacteria can cause new, smaller erythema migrans-like rashes to appear on different parts of the body.
Facial palsy (Bell's palsy): Weakness or paralysis of one or both sides of the face is a common neurological symptom in this stage, affecting approximately 5% of patients.
Severe headaches and neck stiffness: These can be signs of meningitis, an inflammation of the membranes surrounding the brain and spinal cord.
Heart palpitations (Lyme carditis): The bacteria can affect the heart, leading to irregular heartbeats, chest pain, or dizziness. This occurs in about 4-10% of untreated cases in the US and 0.3-4% in Europe. In serious cases, it can cause heart block.
Nerve pain: Burning, shooting pains, numbness, or tingling in the limbs can occur as the bacteria affect the peripheral nervous system. This is part of neuroborreliosis, which affects 10-15% of untreated individuals.
Stage 3: Late Disseminated Infection and Complications
This stage can occur months or years after infection if borreliosis disease remains untreated. The bacteria can cause chronic inflammation and damage to various body systems, leading to debilitating long-term consequences.
Key complications in this stage include:
Lyme arthritis: This is the most common late-stage manifestation in the U.S., affecting up to 60% of untreated individuals. It typically involves episodes of severe joint pain and swelling, most commonly in large joints like the knees. These episodes can recur over months or years.
Neurological problems (Lyme neuroborreliosis): Chronic neurological issues can develop, including:
Cognitive issues (brain fog): Problems with memory, concentration, and mental clarity are frequently reported.
Numbness in extremities: Persistent numbness, tingling, or weakness in the hands, feet, or other areas.
More severe manifestations can include encephalopathy (brain dysfunction) leading to sleep disorders and depression.
Acrodermatitis chronica atrophicans (ACA): This is a rare, chronic skin condition primarily seen in European cases. It causes thinning and discoloration of the skin, usually on the backs of the hands and feet, and can lead to permanent skin damage.
While these complications are serious, they are largely preventable with timely and appropriate treatment in the earlier stages.
Diagnosis and Standard Treatment Protocols
Diagnosing borreliosis disease can be challenging as its symptoms overlap with other conditions. At Greenland Medical, we emphasize a thorough clinical evaluation, including patient history (like tick exposure) and a physical exam. The presence of an erythema migrans rash in an endemic area is often sufficient for a clinical diagnosis in the early stage.
However, for later stages or when the rash is absent, laboratory tests become crucial. We always refer to established guidelines, such as the CDC guidelines on diagnosis and testing, to ensure accurate and reliable results.
How Borreliosis is Diagnosed
The CDC recommends a two-step serologic testing process for borreliosis disease to increase accuracy and reduce false positives. This process involves:
Enzyme Immunoassay (EIA) or ELISA test: This is the initial screening test. It detects antibodies to Borrelia burgdorferi in your blood. If this test is negative, no further testing is usually recommended unless there's a strong clinical suspicion of early infection where antibodies may not yet be present.
Western blot: If the EIA/ELISA test is positive or equivocal, a Western blot test is performed to confirm the results. This test looks for antibodies to specific proteins of the Borrelia bacteria. Both IgM and IgG antibodies are typically tested.
It's important to understand the timing of these tests. Antibodies usually become detectable within 4 to 8 weeks after infection. Therefore, testing too early can lead to a false negative result. Serologic diagnosis is generally more than 80% sensitive for patients with neurological or cardiac manifestations.
The CDC does not recommend certain tests for diagnosis, including urine antigen tests or PCR on urine, as they lack sufficient scientific validation. However, in complex cases with unclear serology, specialized tests like the lymphocyte change test (LTT borrelia) may be considered. PCR can also be useful for detecting bacterial DNA in joint fluid or skin biopsies.
Recommended Treatments for Borreliosis Disease
The good news is that borreliosis disease is highly treatable, especially when caught early. The cornerstone of treatment is antibiotic therapy. The specific antibiotic and duration depend on the stage and severity of the infection:
Early Localized Disease: For the classic erythema migrans rash, oral antibiotics like doxycycline, amoxicillin, or cefuroxime are typically prescribed for a course of 10 to 21 days. Doxycycline is often the first choice for adults and children over 9, while amoxicillin is preferred for children under 9 and pregnant or breastfeeding individuals.
Early Disseminated Disease: If the infection has spread to cause facial palsy, multiple rashes, or early neurological symptoms, oral antibiotics may still be effective, sometimes for a slightly longer duration. For more severe neurological or cardiac involvement, intravenous (IV) antibiotics such as ceftriaxone may be necessary for 14-28 days.
Late Disseminated Disease: Lyme arthritis is usually treated with oral antibiotics for 28 days. If symptoms persist, a second course of oral or IV antibiotics may be given. For chronic neurological manifestations, IV antibiotics might be used, often followed by oral antibiotics.
The prognosis with early treatment is excellent. More than 80% of patients with early borreliosis disease experience complete symptom resolution following the recommended antibiotic course. Prompt treatment not only leads to a quicker recovery but also significantly reduces the risk of developing more serious, late-stage complications.
Post-Treatment Lyme Disease Syndrome (PTLDS)
While most people recover fully after antibiotic treatment for borreliosis disease, a minority (estimated to be between 5% and 20%) may experience persistent symptoms. This condition is known as Post-Treatment Lyme Disease Syndrome (PTLDS).
Symptoms of PTLDS can include:
Lingering fatigue
Widespread pain (muscle and joint aches)
Cognitive complaints, often described as "brain fog," affecting memory and concentration
Sleep disturbances
Headaches
The exact cause of PTLDS is not fully understood. It is generally believed that these symptoms are not due to a persistent, active Borrelia infection that requires more antibiotics. Instead, hypotheses include residual damage to tissues or the nervous system, ongoing immune activation or autoimmune responses triggered by the initial infection, or even undiagnosed co-infections.
The management of PTLDS focuses on symptom control and supportive care. Prolonged antibiotic therapy for PTLDS is not supported by current scientific evidence and carries its own risks, such as antibiotic resistance and side effects. At Greenland Medical, we understand the frustration of persistent symptoms. Our functional medicine approach aims to identify and address underlying imbalances that may contribute to PTLDS, focusing on immune system support, inflammation reduction, and holistic well-being.
Prevention, Related Conditions, and Outlook
Preventing borreliosis disease is always our first and best strategy. We advocate for a proactive approach that combines personal protection with environmental awareness. By taking simple precautions, you can significantly reduce your risk of tick bites and, consequently, the chances of contracting borreliosis.
Here are some key prevention strategies we recommend:
Use effective insect repellents: Apply EPA-registered insect repellents containing DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone to exposed skin. For clothing and gear, consider products with 0.5% permethrin. Always follow product instructions, and note that products with OLE or PMD are not recommended for children under 3.
Wear protective clothing: When in wooded or grassy areas, wear long-sleeved shirts, long pants, and closed-toe shoes. Tuck your pant legs into your socks to create a barrier. Light-colored clothing makes it easier to spot ticks.
Perform daily tick checks: After spending time outdoors, thoroughly check your body for ticks. Pay close attention to areas like your underarms, hair, hairline, ears, waist, groin area, behind the knees, and inside the bellybutton. A mirror can be helpful for hard-to-see spots.
Shower soon after outdoor activities: Showering within a few hours of coming indoors can help wash off loose ticks before they have a chance to attach.
Heat treat clothing: Ticks can survive a wash cycle. After outdoor activities, put your clothes in a dryer on high heat for at least 10 minutes to kill any lingering ticks.
Check pets: If your pets spend time outdoors, inspect them daily for ticks. Consult your veterinarian for tick prevention products suitable for your animals.
Stay on clear paths: When hiking or walking in nature, stick to designated trails and avoid walking through tall grass, brush, or leaf litter.
Landscape management: If you live in a tick-prone area, consider modifying your yard to make it less tick-friendly. This includes clearing tall grass, brush, and leaf litter, and creating wood chip or gravel barriers between wooded areas and your lawn.
How to Prevent Borreliosis Disease
As mentioned, effective prevention is a multi-pronged approach. We encourage everyone to make tick awareness a part of their outdoor routine.
Use insect repellent (DEET or picaridin): These are highly effective for direct skin application. Permethrin-treated clothing and gear offer additional protection, as permethrin kills ticks on contact.
Wear protective clothing: Long sleeves and pants, especially tucked into socks, create a physical barrier against ticks.
Perform daily tick checks: A thorough head-to-toe check, including hair, skin folds, and behind the ears, is essential after any outdoor activity. Prompt removal is key. The bacteria are less likely to spread borreliosis disease if you remove the tick within 24 hours.
If you find an attached tick, here’s how to remove it correctly:

Use fine-tipped tweezers: Grasp the tick as close to the skin's surface as possible.
Pull upward with steady, even pressure: Don't twist or jerk the tick; this can cause the mouthparts to break off and remain in the skin.
Clean the bite area: After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
Avoid folk remedies: Do not use heat, petroleum jelly, nail polish, or other methods to remove the tick. These can irritate the tick and cause it to release more bacteria into the bite wound.
Landscape management (clear brush, keep grass short): Creating a "tick-safe zone" around your home can also help. Ticks prefer moist, shady environments. By keeping your lawn mowed, clearing leaf litter, and creating a buffer zone of wood chips or gravel between your yard and wooded areas, you can deter ticks.
Related Conditions and Co-infections
Borreliosis disease is complex, and it's important to recognize that different Borrelia species exist, causing variations in symptoms and geographical distribution. For instance, while Borrelia burgdorferi is the main species in the US, Borrelia afzelii often causes skin manifestations in Europe, and Borrelia garinii is more commonly associated with neurological symptoms there. There's also Borrelia mayonii, a newer species identified in the US, and Borrelia miyamotoi, which can cause a relapsing fever-like illness.
Furthermore, ticks can carry more than one pathogen, leading to tick-borne co-infections. If a tick is infected with multiple types of bacteria or parasites, a single bite can transmit more than one disease. Common co-infections with borreliosis include:
Babesiosis: Caused by Babesia parasites, this infection can cause flu-like symptoms, fatigue, and hemolytic anemia. It can be particularly severe in immunocompromised individuals.
Anaplasmosis: Caused by Anaplasma phagocytophilum bacteria, anaplasmosis can lead to fever, headache, muscle aches, and low white blood cell and platelet counts. We have a detailed review on Anaplasmosis in Europe for those interested in learning more.
Co-infections can complicate diagnosis and treatment, often leading to more severe or persistent symptoms than borreliosis alone. This is why a comprehensive diagnostic approach is crucial, especially in patients with atypical or refractory symptoms.
What is the Outlook for Individuals with Borreliosis?
The outlook for individuals diagnosed with borreliosis disease is generally excellent, especially with early detection and appropriate antibiotic treatment. Most people recover fully and experience complete resolution of their symptoms. Studies show that over 80% of patients treated in the early stages achieve full recovery.
Even in later stages, antibiotic treatment can effectively resolve symptoms, though the recovery process might be longer and require more intensive therapy (e.g., intravenous antibiotics). While untreated borreliosis can lead to serious complications affecting the joints, heart, and nervous system, it is rarely fatal.
However, as we've discussed, a minority of individuals may develop Post-Treatment Lyme Disease Syndrome (PTLDS), experiencing lingering symptoms like fatigue, pain, and cognitive issues. While challenging, PTLDS is not an indication of ongoing infection, and its management focuses on addressing the persistent symptoms and supporting the body's healing. At Greenland Medical, we specialize in supporting individuals through these complex, chronic conditions, seeking to address underlying imbalances that may contribute to prolonged symptoms.
Frequently Asked Questions about Borreliosis
We understand that borreliosis disease can raise many questions. Here, we address some of the most common inquiries we receive:
Can borreliosis be transmitted from person to person?
No, there is no evidence that borreliosis disease can be transmitted from person to person through casual contact like touching, kissing, or sexual contact. It is also not spread through the air, food, or water. While congenital transmission from a pregnant mother to her fetus is theoretically possible, it has not been conclusively proven and is considered very rare, with no documented cases of severe outcomes for the baby.
Is there a vaccine for borreliosis?
Currently, there is no human vaccine for Lyme disease widely available in the United States. A previous vaccine, LYMERix, was available from 1998 to 2002 but was voluntarily discontinued by its manufacturer due to low demand and public concerns (despite being deemed safe and effective by health authorities).
However, research into new vaccines is ongoing, with several candidates in various stages of development. Scientists are exploring different approaches, including traditional protein-based vaccines and newer mRNA vaccine technologies. We remain hopeful that a new, effective vaccine will become available in the future to offer another layer of protection against borreliosis disease.
What happens if borreliosis is left untreated?
If borreliosis disease is left untreated, the Borrelia bacteria can spread throughout the body, leading to more severe and chronic health problems. The infection can spread from the initial skin rash to affect multiple organ systems, including:
Joints: Leading to Lyme arthritis, characterized by recurrent episodes of painful swelling, most commonly in the knees. In up to 60% of untreated people, Lyme arthritis can develop.
Heart: Causing Lyme carditis, which can lead to heart palpitations, dizziness, and serious heart rhythm abnormalities, including heart block. This occurs in about 4-10% of untreated cases in the United States.
Nervous system: Resulting in neuroborreliosis, which can manifest as facial nerve paralysis (Bell's palsy), meningitis (inflammation of the brain and spinal cord membranes), nerve pain, numbness, tingling, and cognitive difficulties like brain fog. Neurological complications occur in around 10-15% of untreated cases.
These late-stage manifestations are significantly more difficult to treat than early-stage borreliosis disease and can lead to prolonged suffering and potential long-term damage. This underscores the critical importance of early diagnosis and treatment.
Conclusion: A Proactive Approach to a Complex Illness
We've covered a lot of ground in understanding borreliosis disease, from its microscopic origins in Borrelia bacteria and tick vectors to its varied symptoms, diagnostic challenges, and effective treatments. The key takeaways are clear: borreliosis is a serious but treatable infection, and early recognition and prevention are paramount.
By being vigilant about tick exposure, practicing effective prevention strategies, and seeking prompt medical attention if symptoms arise, you can significantly reduce your risk and improve your outcome.
For those who have steerd the complexities of borreliosis disease and continue to experience lingering symptoms, or for individuals struggling with other complex chronic conditions, we understand the frustration when conventional approaches fall short. At Greenland Medical, we believe in going beyond symptom management to find and fix the root causes of illness. We use a functional medicine approach, combining modern and natural therapies, including advanced protocols, to create personalized health strategies. Our goal is to support your body's innate healing abilities and help you regain your vitality.
