
Beyond the Hype: What You Need to Know About Allergy Test Reliability
Why Understanding Test Accuracy Could Save Your Health
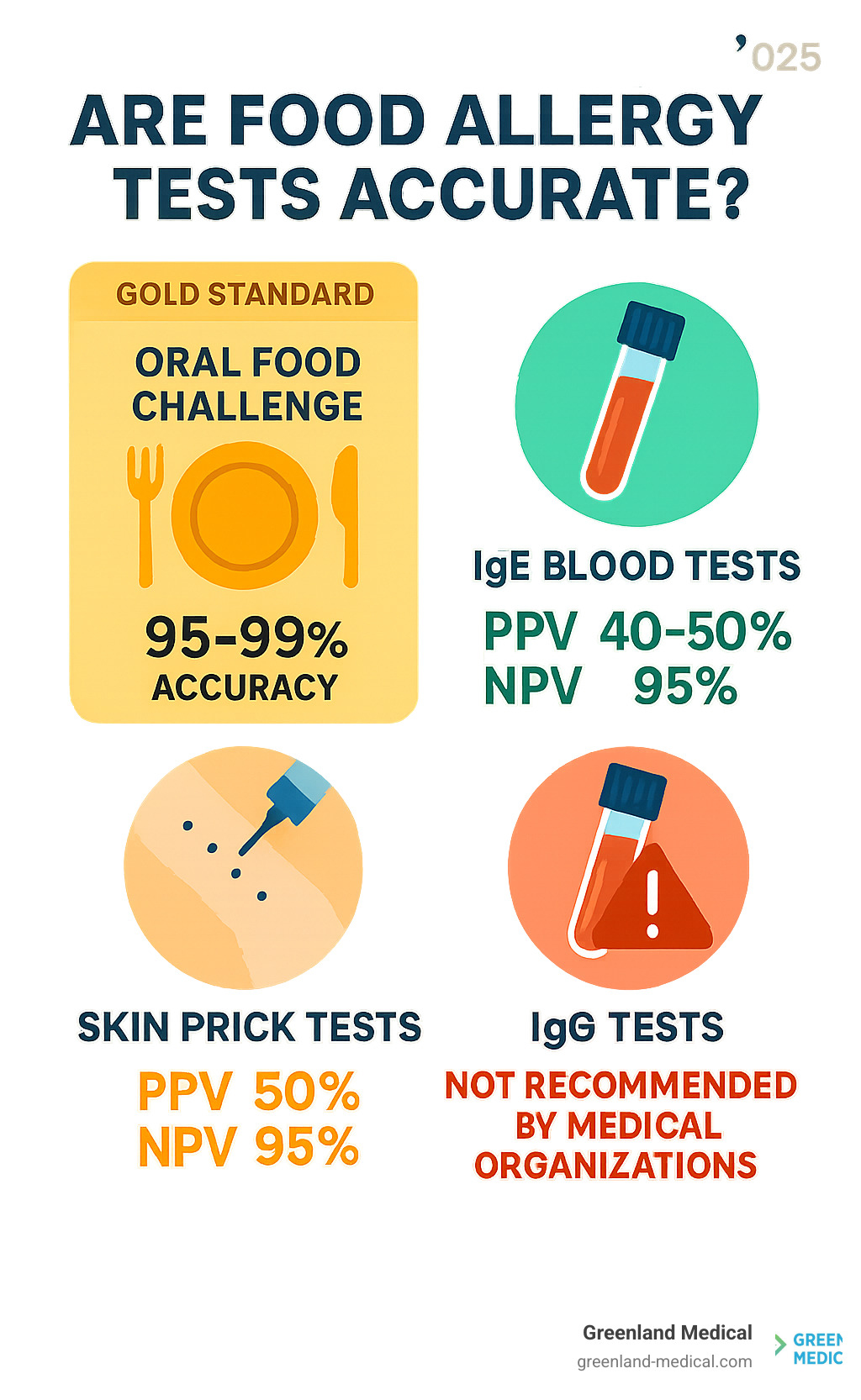
Are food allergy tests accurate? This question matters more than you might think. The short answer is: it depends entirely on which test you're using and who's interpreting the results.
Quick Answer:
IgE blood tests and skin prick tests: 50-60% false positive rate, but 95% accurate when negative
At-home IgG "sensitivity" tests: Not recommended by medical organizations - measure tolerance, not allergy
Oral Food Challenge: Gold standard with highest accuracy when medically supervised
Medical history + validated testing: Most reliable approach for diagnosis
If you've ever wondered whether that expensive at-home food sensitivity test is worth it, or why your doctor seems skeptical about your "positive" results, you're not alone. Many people spend hundreds of dollars on tests that major medical organizations actively warn against.
The stakes are higher than wasted money. Unreliable tests can lead to unnecessary food restrictions, nutritional deficiencies, and missed diagnoses of serious conditions. Even worse, some tests give false reassurance to people with genuine allergies.
I'm Dr Andrew Greenland, and in my functional medicine practice, I regularly see patients who've been misled by inaccurate food allergy tests, leading to years of unnecessary dietary restrictions and continued symptoms. Understanding which tests are food allergy tests accurate is crucial for getting the right diagnosis and treatment approach.
Allergy, Intolerance, or Sensitivity? Understanding Your Body's Reaction
Before we dive into whether are food allergy tests accurate, we need to clear up some confusion. Most people use "food allergy," "food intolerance," and "food sensitivity" as if they mean the same thing. They don't – and mixing them up can lead you down the wrong path entirely.
Think of it this way: your body has different ways of saying "I don't like this food." Some are whispers, others are screams, and some are false alarms altogether.
Food allergies are your body's emergency response system gone haywire. When you have a true food allergy, your immune system treats a harmless food protein like a dangerous invader. It creates specific antibodies called IgE antibodies that launch an immediate counterattack.
This isn't subtle. We're talking about hives breaking out within minutes, your lips or tongue swelling up, or even anaphylaxis – a life-threatening reaction that can make it impossible to breathe. Even tiny amounts of the trigger food can set this off. About 8% of children have genuine food allergies, and the numbers keep climbing in Western countries.
The usual suspects? Milk, eggs, peanuts, tree nuts, fish, shellfish, soy, and wheat top the list.
Food intolerance is more like your digestive system throwing a tantrum. Unlike allergies, your immune system isn't involved at all. Instead, your body simply lacks the right tools to break down certain foods properly.
Lactose intolerance is the perfect example. Your body doesn't make enough lactase enzyme to digest milk sugar, so you end up with bloating, gas, stomach pain, and diarrhea. These symptoms can take hours or even days to show up, and while they're miserable, they won't land you in the emergency room.
Food sensitivity is where things get murky. This term gets thrown around a lot, often referring to delayed reactions that might involve IgG antibodies instead of IgE. Supporters claim these reactions cause everything from brain fog and joint pain to headaches and fatigue.
Here's the problem: mainstream medical organizations don't recognize IgG testing as a valid way to diagnose food problems. As we'll explore later, these tests often measure your body's tolerance to foods, not your sensitivity to them.
Understanding these differences isn't just academic – it's crucial for getting the right diagnosis and treatment. Confusing a food intolerance with an allergy could leave you carrying an unnecessary EpiPen. Mistaking normal IgG responses for food sensitivities could have you eliminating perfectly healthy foods from your diet.
When patients come to me with a bag full of test results claiming they're "allergic" to 20 different foods, the first thing we do is sort out what type of reaction they're actually having. Only then can we figure out which tests might actually help – and which ones are just expensive guesswork.
For a deeper dive into the science behind food intolerances, check out this comprehensive review on food intolerance.
The Unreliability of At-Home & Unproven "Sensitivity" Tests
If you've been dealing with mysterious symptoms like chronic fatigue, brain fog, or ongoing digestive issues, you've probably stumbled across those tempting at-home food "sensitivity" tests. They're everywhere online, promising to solve your health puzzles with just a simple blood or hair sample sent from your kitchen table.
Here's what I need you to know: these tests are widely considered unreliable by medical professionals, and using them could actually make your health journey more confusing and expensive.

The most popular type of at-home test measures something called IgG antibodies to various foods. The marketing sounds convincing: high levels of these antibodies supposedly indicate you're "sensitive" to those foods, and eliminating them will magically fix your symptoms.
But here's the problem - IgG antibodies are actually a sign that your immune system is working normally. When you eat foods regularly, your body naturally produces these antibodies as part of healthy immune tolerance. It's like your immune system keeping a friendly record of foods it recognizes, not sounding an alarm about foods that are harming you.
Think about it this way: if you eat bread every day, you'll likely have IgG antibodies to wheat. That doesn't mean wheat is making you sick - it means your body knows wheat and is handling it just fine.
The American Academy of Allergy, Asthma & Immunology strongly warns against IgG testing for food allergies or intolerances. Their position on IgG testing is crystal clear: these tests don't work for diagnosing food problems.
Why are these tests so problematic? First, they fundamentally misunderstand what IgG antibodies mean. Everyone who eats a normal diet will have IgG antibodies to their regular foods - that's completely normal and healthy.
Second, there's no scientific evidence linking IgG levels to actual symptoms. The studies that companies cite to support these tests are often poorly designed and don't meet basic scientific standards.
Third, these tests often flag dozens of foods as "problematic," leading people to eliminate huge portions of their diet unnecessarily. I've seen patients told to avoid 20 or more foods based on these tests, including nutritional staples like eggs, wheat, and dairy.
Perhaps most concerning is how inconsistent these tests are. Send the same blood sample to two different companies, and you'll likely get completely different results. That's not how accurate medical testing works.
The consequences of relying on these unproven tests can be serious. Unnecessary elimination diets can lead to nutritional deficiencies and make social eating incredibly stressful. Some people develop genuine anxiety around food, constantly worrying about what they can and can't eat based on misleading information.
Even more dangerous, these tests can provide false reassurance to people with real food allergies, potentially leading them to consume foods that could trigger life-threatening reactions.
There are other unproven methods floating around too. Applied Kinesiology claims to detect food problems by testing muscle weakness when you hold suspected allergens. Electrodermal testing measures electrical currents in your body while exposed to potential allergens. Neither has any scientific basis.
The bottom line? When you're wondering "are food allergy tests accurate," the answer depends entirely on which test you're considering. At-home IgG tests and other unproven methods simply aren't reliable tools for understanding your body's relationship with food.
Your symptoms deserve proper investigation, but these tests are more likely to send you down the wrong path than provide real answers. The money you'd spend on unproven testing would be much better invested in working with a qualified healthcare provider who can help identify what's really going on.
Are Food Allergy Tests Accurate? A Guide to Medically-Approved Methods
When it comes to answering the question, "are food allergy tests accurate?", we must turn to medically approved and scientifically validated methods. These tests, combined with a detailed medical history and clinical evaluation by an allergist, form the cornerstone of an accurate diagnosis.
Our approach at Greenland Medical always begins with a comprehensive medical history. We'll ask about your symptoms, when they occur, what you've eaten, and any family history of allergies. Keeping a detailed food and symptom journal can be incredibly helpful for this stage, providing us with crucial clues. This initial consultation helps us determine which specific tests are most appropriate for your situation.
The most reliable methods for diagnosing food allergies involve looking for IgE antibodies, which are the immune system's immediate response to allergens.
Skin Prick Tests (SPT): What Do the Results Mean?
The Skin Prick Test (SPT) is one of the most common and valuable tools allergists use.
How SPT works: A small amount of liquid containing a suspected food allergen is placed on your skin, typically on your forearm or back. The skin is then gently pricked or scratched through the liquid, allowing the allergen to enter just beneath the surface.
IgE sensitization: If you are allergic to that food, your immune system's IgE antibodies will react with the allergen, triggering a localized response.
Wheal and flare: Within 15-20 minutes, a positive reaction will appear as a raised, red, itchy bump (a "wheal") surrounded by a red flush (a "flare"). The size of the wheal can indicate the degree of sensitization, but it does not predict the severity of a potential allergic reaction.
Limitations: While SPTs are quick and relatively inexpensive, they have limitations. A positive SPT is reliable about 50 percent of the time, meaning that 50-60% of tests can give a false positive. This means about half of people who test positive on a skin prick test don’t actually have an allergic reaction to that food. A positive result indicates sensitization (the presence of IgE antibodies), but not necessarily a clinical allergy (meaning you would react if you ate the food).
High negative predictive value: However, a negative SPT result is about 95 percent predictive. This means that if an SPT is negative, it's highly unlikely you have an IgE-mediated allergy to that food.
Not a standalone diagnosis: Due to the possibility of false positives, SPT results must always be interpreted in conjunction with your medical history and clinical symptoms. We often advise patients to stop taking antihistamines five days before an SPT, as these medications can interfere with the test results.
IgE Blood Tests: When are food allergy tests accurate with blood samples?
IgE blood tests (also known as specific IgE blood tests or RAST tests, though newer versions like ImmunoCAP are more common) measure the amount of IgE antibodies to specific foods circulating in your blood.
How IgE blood tests work: A blood sample is taken and sent to a lab, where it's tested against various food allergens. The lab measures the quantity of food-specific IgE antibodies. Results are typically reported as a numerical value, often falling into different "classes" based on the level of IgE detected.
When to use: These tests are particularly useful when skin prick testing isn't feasible, such as for individuals with severe eczema covering large areas of their skin, or for those who cannot stop taking antihistamines or other medications that might interfere with SPT results.
Limitations: Similar to SPTs, IgE blood tests can have a significant false positive rate. RAST has a slightly higher false positive rate than SPT, making it less reliable for confirming an allergy. While they can indicate sensitization, a positive result doesn't always mean a clinical allergy. The level of IgE antibodies does not necessarily predict the severity of a reaction. Furthermore, IgE tests don’t test for all kinds of allergies, because not all food allergies are based on food-specific IgE response. For instance, Food Protein-Induced Enterocolitis Syndrome (FPIES) is an allergic reaction that does not involve IgE antibodies.
Atopy Patch Testing (APT): For Delayed Reactions
While SPTs and IgE blood tests primarily detect immediate, IgE-mediated reactions, some food-related conditions involve delayed, cell-mediated immune responses that don't produce IgE antibodies. This is where Atopy Patch Testing (APT) can sometimes be used.
Delayed cell-mediated reactions: APT is designed to detect these non-IgE mediated reactions, which can manifest hours or even days after exposure.
Non-IgE allergies: APT is sometimes used to help diagnose conditions like Eosinophilic Esophagitis (EoE) and Food Protein-Induced Enterocolitis Syndrome (FPIES), where standard IgE tests are often negative despite a clear adverse reaction to food.
How APT works: Small patches containing suspected food allergens are applied to the skin, usually on the back, and left in place for 48 to 72 hours. The skin is then examined for any delayed reactions, such as redness, swelling, or small blisters.
Limitations: APT is less standardized than SPT or IgE blood tests, and its interpretation requires significant expertise. It is not widely used for general food allergy diagnosis but can be a valuable tool in specific clinical scenarios, helping us pinpoint triggers for these unique, delayed immune responses.
The Gold Standard: The Oral Food Challenge (OFC)

When patients ask me "are food allergy tests accurate?" I always explain that while skin tests and blood work are valuable tools, there's one test that stands above all others for accuracy: the Oral Food Challenge (OFC). Think of it as the ultimate truth test for food allergies.
The OFC is considered the gold standard because it's the only test that directly measures what really matters - whether you actually react when you eat the food. While other tests can show sensitization (having antibodies), only the OFC reveals if those antibodies translate into real-world symptoms.
Here's why the OFC is so definitive: Instead of looking for markers in your blood or on your skin, we actually give you the suspected food in a carefully controlled medical environment. It's like the difference between asking someone if they can drive versus watching them behind the wheel.
The process is methodical and safe. After you've avoided the suspected food for a period of time, we start with tiny amounts - sometimes as small as a few milligrams. Every 15 to 30 minutes, we gradually increase the dose while monitoring you closely for any signs of reaction. The entire process typically takes several hours.
Safety is our top priority during every OFC. This isn't something you should ever attempt at home - it must be conducted in a medical setting with trained allergists and emergency equipment immediately available. We monitor your vital signs throughout, and if any reaction occurs, we stop the challenge immediately and provide appropriate treatment.
We use the OFC in several key situations. Sometimes patients have positive skin or blood tests but no clear history of reactions - the OFC helps us determine if there's a true clinical allergy. It's also invaluable for checking if children have outgrown their food allergies, which happens frequently with milk and egg allergies. In some cases, we can even determine a threshold dose that you can safely tolerate.
The results are remarkably clear-cut. If you can eat increasing amounts of the food without any reaction, you're not allergic. If you do react, we have our definitive answer - and we're right there to manage it safely.
The OFC does require time and carries some risk since we're intentionally exposing you to a potential allergen. That's why we reserve it for situations where we really need that definitive answer. For more detailed information about what to expect, Food Allergy Research & Education provides comprehensive resources on the Oral Food Challenge.
While the OFC is the most accurate single test available, the best diagnostic approach still combines it with a thorough medical history and clinical evaluation. That's how we ensure you get the most reliable answers about your food reactions.
Frequently Asked Questions about Food Allergy Testing
You're not alone if food allergy testing feels overwhelming. We hear these same questions from patients every day, and honestly, the confusion is completely understandable given all the mixed messages out there.
What is the most reliable test for food allergies?
Here's the thing that might surprise you: are food allergy tests accurate when used alone? Not really. The most reliable approach isn't actually a single test at all.
Think of diagnosing a food allergy like solving a puzzle. Your detailed medical history is the biggest piece of that puzzle. If you consistently break out in hives every time you eat shrimp, that story often matters more than any test result. We call this the "cornerstone of diagnosis" for good reason.
IgE tests - whether through skin pricks or blood draws - add important pieces to the puzzle. They show us if your immune system recognizes specific foods as threats. A negative result is incredibly reliable (95% accurate), so if it's negative, you can breathe easy knowing you likely don't have that allergy.
But here's where it gets tricky: positive results need careful interpretation. 50-60% false positive rate we mentioned? This is why you need an allergist's expertise to make sense of everything.
The Oral Food Challenge remains our gold standard when we need absolute certainty. It's like the final piece that completes the puzzle, showing us exactly how your body responds to a food in real life.
The magic happens when we put all these pieces together. Your story, the test results, and expert medical interpretation create a complete picture that's far more reliable than any single test could ever be.
Can a food allergy test be wrong?
Absolutely, and this is exactly why we emphasize that comprehensive approach. Food allergy tests can definitely be wrong, and understanding this helps you make better decisions about your health.
False positives are surprisingly common with IgE tests. Your skin might react to a prick test, or your blood might show IgE antibodies to peanuts, but you could eat peanut butter sandwiches all day without any problems. This happens because your immune system recognizes the food but doesn't actually cause symptoms - we call this "sensitization without clinical reactivity."
It's like your immune system saying "I know this food" without necessarily saying "I don't like this food."
False negatives are less common with properly conducted IgE tests, but they can happen. You might have very low levels of sensitivity, or your allergy might work through a different immune pathway that IgE tests don't catch.
Now, those IgG tests we discussed earlier? They're consistently wrong when it comes to diagnosing allergies. They measure normal immune tolerance, not allergic reactions. It's not that the test itself is technically faulty - it's that what it measures has nothing to do with food allergies.
This is exactly why we never rely on test results alone. Every result needs to be weighed against your actual experiences with food.
When should I see a doctor for a suspected food allergy?
Trust your instincts here. If something feels wrong after eating, it's worth investigating properly.
Seek immediate medical attention if you experience hives, swelling of your face or throat, trouble breathing, or dizziness after eating. These could signal anaphylaxis, which is a medical emergency that requires immediate treatment.
Make an appointment soon if you notice consistent patterns - like stomach pain every time you have dairy, or a rash that appears after eating eggs. Even if the symptoms seem mild, getting clarity helps you make informed decisions about your diet.
Consider a consultation if you're dealing with chronic symptoms like persistent fatigue, brain fog, joint pain, or ongoing digestive troubles that haven't responded to other treatments. While these might not be food allergies, a functional medicine approach can help identify root causes that traditional medicine sometimes misses.
Don't wait if you need guidance on managing a suspected allergy. Understanding whether you need an epinephrine auto-injector, knowing which foods to avoid, and learning how to read labels properly can be life-changing - and sometimes life-saving.
Your primary care doctor can often provide initial guidance and refer you to an allergist when needed. At Greenland Medical, we take a comprehensive approach that looks at your whole health picture, not just isolated symptoms, to help you get to the root of what's really going on.
Getting to the Root Cause of Your Symptoms
After exploring the complex world of food allergy testing, I hope one thing is crystal clear: are food allergy tests accurate? The answer depends entirely on which tests you choose and who interprets them.
The unreliability of IgG testing cannot be overstated. These expensive at-home "sensitivity" tests that promise to revolutionize your health by identifying dozens of problem foods are simply not backed by science. Major medical organizations worldwide warn against them because IgG antibodies actually indicate tolerance to foods, not sensitivity. Yet these tests continue to lead people down rabbit holes of unnecessary food restrictions and nutritional deficiencies.
Your medical history remains the cornerstone of accurate diagnosis. The story of when, where, and how you react to foods provides invaluable clues that no test can replace. This is why keeping a detailed food and symptom journal can be so powerful—it helps paint the complete picture of what's really happening in your body.
When it comes to validated testing methods, the medically approved options we've discussed—skin prick tests, IgE blood tests, and the gold standard oral food challenge—offer real diagnostic value when interpreted by qualified allergists. Yes, they have limitations, particularly with false positives, but they're based on solid science and decades of clinical experience.
At Greenland Medical, we see many patients who've spent months or even years following restrictive diets based on unreliable tests, only to find their symptoms persist. That's because many chronic symptoms that seem like food reactions actually stem from deeper root causes. Issues like gut dysbiosis, chronic inflammation, nutrient deficiencies, or hormonal imbalances can create symptoms that mimic food sensitivities.
Our functional medicine approach looks beyond surface-level symptoms to identify these underlying imbalances. Rather than simply eliminating foods based on questionable test results, we work to understand why your body might be reacting in the first place. Sometimes addressing gut health, reducing inflammation, or supporting your body's natural detoxification processes can resolve symptoms without requiring you to avoid perfectly healthy foods.
This doesn't mean we dismiss genuine food allergies or intolerances—quite the opposite. We believe in using scientifically sound methods to identify real food reactions while simultaneously addressing the root causes that might be contributing to your symptoms.
If you're tired of playing guessing games with your health, following restrictive diets that don't work, or dealing with persistent symptoms that no one seems able to explain, we're here to help. Our team combines the best of modern diagnostic methods with natural therapies to create personalized treatment plans that actually address what's happening in your unique body.
Explore our approach to food allergy and sensitivity testing to learn how we can help you find the clarity and relief you've been searching for. Because when it comes to your health, you deserve answers that are both accurate and actionable.
